Sketchy Botox shots spark multistate outbreak of botulism-like condition
Yikes —
So far at least six people in two states have fallen ill; four of them were hospitalized.

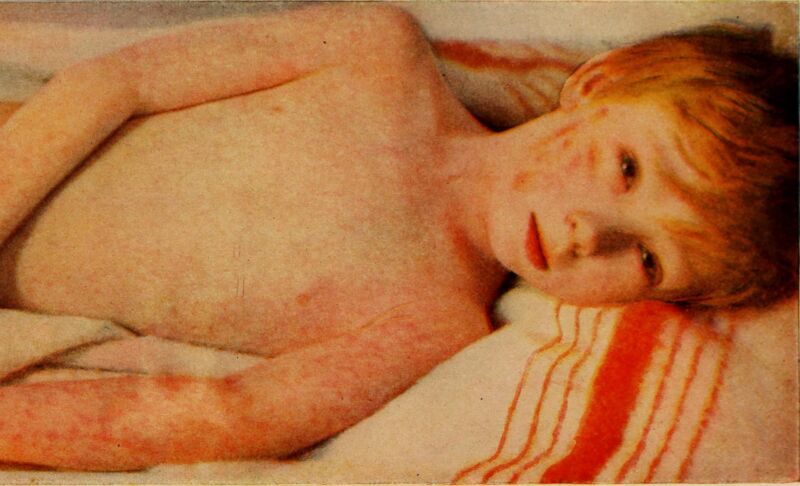
Enlarge / A woman in New Jersey receiving a Botox treatment at a Botox party in a New Jersey salon hosted by a radio station.
Sketchy cosmetic injections of what seem to be counterfeit Botox are behind a multistate outbreak of botulism-like illnesses, state health officials report.
So far, at least six people have fallen ill in two states: four in Tennessee and two in Illinois. Four of the six people required hospitalization for their condition (two in Tennessee and both cases in Illinois).
The Centers for Disease Control and Prevention is reportedly planning to nationwide alert to notify clinicians of the potentially counterfeit Botox and advise them to be on the lookout for botulism-like illnesses. The agency did not immediately respond to Ars’ request for information.
Botox is a regulated drug product that contains purified, controlled quantities of the botulinum neurotoxin, which is made by certain Clostridium bacterial species, especially Clostridium botulinum. The toxin causes muscle paralysis by blocking the release of a neurotransmitter. When people are exposed to the toxin from wound infections or by accidentally eating contaminated foods, it can lead to full paralysis, including in muscles used for breathing. But, the toxin can also be used safely for cosmetic procedures to smooth facial wrinkles—when well-regulated and approved doses administered by licensed medical professionals are used.
All of those important conditions for use did not seem to be met in the cases identified so far. Tennessee reported that its four cases were linked to injections given in “non-medical settings such as homes or cosmetic spas.” Investigators found that the injections were of “products with unclear origin” and that information collected so far suggests the products were counterfeit.
The two people sickened in Illinois, meanwhile, both received injections from a nurse in LaSalle County who was “performing work outside her authority.” State officials said the injections were of Botox or a similar, possibly counterfeit product.
The early symptoms of botulism can include double or blurred vision, drooping eyelids, slurred speech, difficulty swallowing, dry mouth, and difficulty breathing, Tennessee health officials noted. After that, people may suffer descending, symmetric muscle weakness that progresses over hours to days, requiring hospitalization and treatment with an anti-toxin.
Illinois officials reported that the cases reported similar symptoms, such as blurred or double vision, droopy face, fatigue, shortness of breath, difficulty breathing, and a hoarse voice, after getting their injections.
“Illinois residents should exercise caution when considering cosmetic treatment,” Illinois Department of Public Health Director Sameer Vohra said in a statement. “Receiving these treatments in unlicensed, unapproved settings can put you or your loved ones at serious risk for health problems. Please only seek cosmetic services under the care of licensed professionals trained to do these procedures and who use FDA approved products. If you are experiencing any health problems after a recent cosmetic treatment, please contact your healthcare provider immediately for help and assistance.”
Sketchy Botox shots spark multistate outbreak of botulism-like condition Read More »