People are seizing, being intubated after eating microdose chocolates
Yikes —
“Extreme caution” urged as at least 8 people in 4 states sickened, 6 hospitalized.
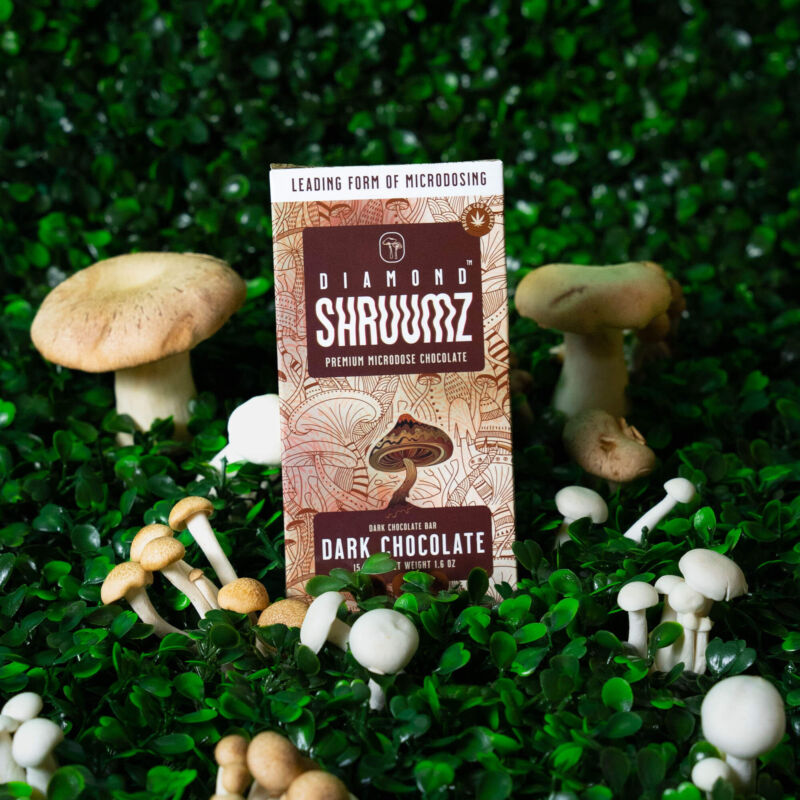
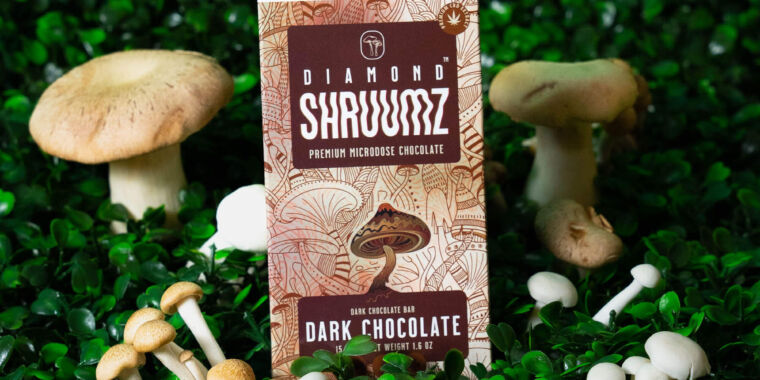
Enlarge / A Diamond Shruumz chocolate bar, which come in a variety of flavors.
Various federal and state health officials are sounding the alarm on Diamond Shruumz-brand Microdosing Chocolate Bars. The candy, said to be infused with mushrooms, has been linked to severe illnesses, including seizures, loss of consciousness, confusion, sleepiness, agitation, abnormal heart rates, hyper/hypotension, nausea, and vomiting, according to an outbreak alert released by the Food and Drug Administration on Friday.
So far, eight people across four states have been sickened—four in Arizona, two in Indiana, one in Nevada, and one in Pennsylvania, the FDA reported. Of the eight, six have been hospitalized.
“We are urging the public to use extreme caution due to the very serious effects of these products,” Maureen Roland, director of the Banner Poison and Drug Information Center in Phoenix, said in a press release earlier this week.
Steve Dudley, director of the Arizona Poison and Drug Information Center, added that there’s “clearly something toxic occurring” with the chocolates. “We’ve seen the same phenomenon of people eating the chocolate bar then seizing, losing consciousness, and having to be intubated.” Dudley noted that the state is aware of additional cases beyond the eight reported Friday by the FDA. Those cases were reported from Nebraska and Utah.
It’s not entirely clear what is in the chocolates or what could be causing the illnesses. The FDA said it was working with the Centers for Disease Control and Prevention as well as America’s Poison Centers to “determine the cause of these illnesses and is considering the appropriate next steps.”
On its website, Diamond Shruumz says that its chocolate bars contain a “primo proprietary blend of nootropic and functional mushrooms.” The website also contains reports of laboratory analyses on their products, some of which indicate the absence of select known fungal toxins and compounds such as the hallucinogen psilocybin and cannabinoids.
Diamond Shruumz did not immediately respond to Ars’ request for comment.
The chocolate bars are still available for sale online but the FDA said that consumers should not eat, sell, or serve them. Any bars already purchased should be discarded. Likewise, retailers should not sell or distribute them. The FDA noted that, in addition to being available online, the bars are also sold in various retail locations nationwide, including smoke/vape shops and retailers that sell hemp-derived products.
People are seizing, being intubated after eating microdose chocolates Read More »