More unidentified illnesses linked to unexplained bird flu case in Missouri
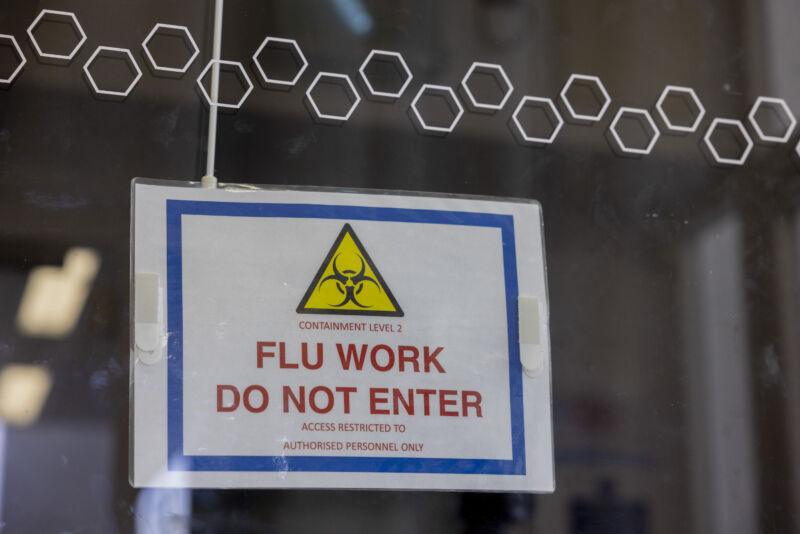
Enlarge / A warning sign outside a laboratory testing the H5N1 bird flu virus at The Pirbright Institute in Woking, UK, on Monday, March 13, 2023.
More than a month after a person in Missouri mysteriously fell ill with H5-type bird flu, investigators in the state are still identifying people who became ill after contact with the patient, raising questions about the diligence of the ongoing health investigation.
On September 6, Missouri’s health department reported the state’s first human case of H5-type bird flu, one that appears closely related to the H5N1 bird flu currently causing a nationwide outbreak among dairy cows. But the infected person had no known contact with infected animals—unlike all of the other 13 human cases identified amid the dairy outbreak this year. Those previous cases have all occurred in dairy- or poultry-farm workers. In fact, Missouri has not reported bird flu in its dairy herds nor recent poultry outbreaks.
Given the unexplained source of infection, health investigators in the state have been working to track the virus both backward in time—to try to identify the source—and forward—to identify any potential onward spread. The bird flu patient was initially hospitalized on August 22 but recovered and had been released by the time the state publicly reported the case.
In an update Friday, September 27, the Centers for Disease Control and Prevention relayed that Missouri officials have now identified four more health care workers who experienced mild respiratory illnesses after caring for the person with bird flu. None of the four workers were tested for flu at the time of their illnesses and all have since recovered.
Testing new cases for antibodies to H5N1
The four newly identified cases bring the total number of health care workers who fell ill after contact to six. Missouri investigators had previously identified two other health care workers who developed mild respiratory symptoms. One of those workers was tested for flu around the time of their illness—and tested negative. But the other, like the four newly identified cases, was not tested. That person has since submitted a blood sample to test for bird flu antibodies, which would indicate a previous infection.
In addition, a household contact of the bird flu patient also fell ill at the same time as the patient, suggesting a possible common source of the infection.
The illnesses are concerning, given the fear that H5N1 bird flu could begin spreading from human to human and spark a widespread outbreak or even a pandemic. However, it can’t be overlooked that a plethora of other respiratory viruses are around—and SARS-CoV-2 transmission was relatively high in Missouri at the time—it’s impossible to draw any conclusions at this point about whether the illnesses were bird flu infections.
But, the illnesses do clearly raise concern about the health investigation, which is being conducted by Missouri officials. “The slow trickle of info is the most concerning part,” infectious disease expert Krutika Kuppalli wrote on social media Friday. The CDC can get involved at the request of a state, but such a request has not been made. For now, the CDC is only providing technical assistance from Atlanta.
In its update today, the CDC emphasized that “to date, only one case of influenza A(H5N1) has been detected in Missouri. No contacts of that case have tested positive for influenza A(H5N1).” The agency added that blood testing results for H5 antibodies are pending.
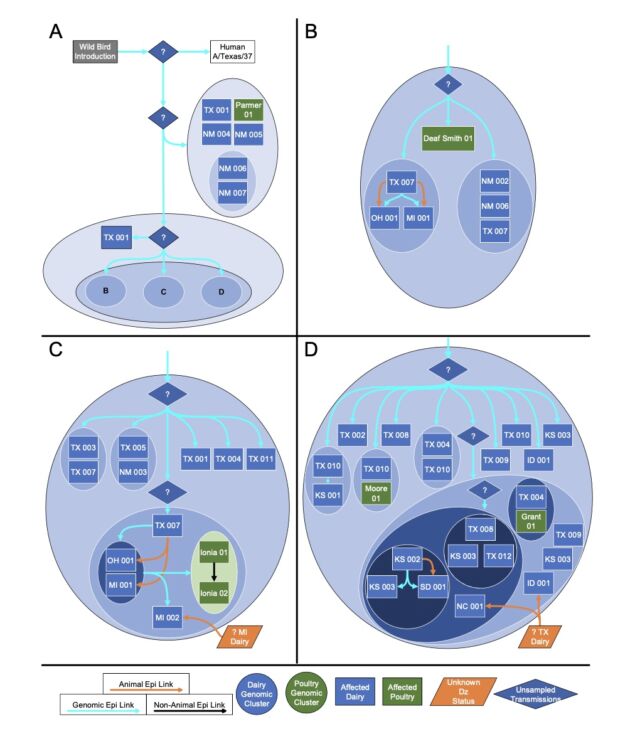
Currently, 239 dairy herds in 14 states have been infected with H5N1.
More unidentified illnesses linked to unexplained bird flu case in Missouri Read More »