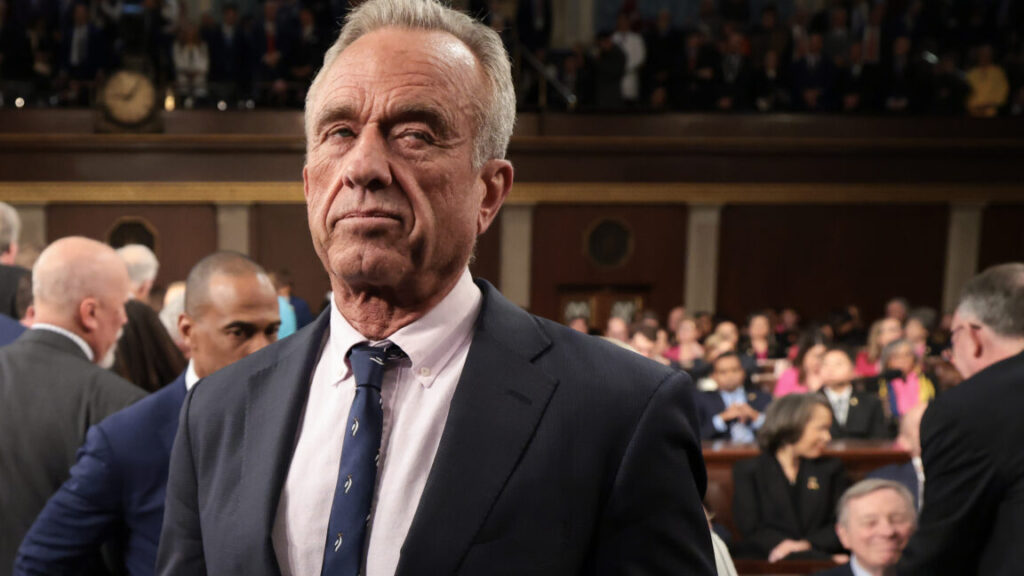
RFK Jr. claws back $11.4B in CDC funding amid wave of top-level departures
Those departures follow Kevin Griffis, head of the CDC’s office of communications, who left last week; Robin Bailey, the agency’s chief operating officer, left late last month; and Nirav Shah, a former CDC principal deputy director.
Pulled funding
Meanwhile, NBC News reported this afternoon that the Department of Health and Human Services (HHS) is pulling back $11.4 billion in funding from the agency, which it allocated to state and local health departments as well as partners.
NBC reported that the funds were largely used for COVID-19 testing and vaccination, and to support community health workers and initiatives that address pandemic health disparities among high-risk and underserved populations, such as rural communities and minority populations. The funds also supported global COVID-19 projects.
“The COVID-19 pandemic is over, and HHS will no longer waste billions of taxpayer dollars responding to a non-existent pandemic that Americans moved on from years ago,” HHS Director of Communications Andrew Nixon said in a statement. “HHS is prioritizing funding projects that will deliver on President Trump’s mandate to address our chronic disease epidemic and Make America Healthy Again.”
State health departments told NBC News that they’re still evaluating the impact of the withdrawn funding. On Monday, some grantees received notices that read: “Now that the pandemic is over, the grants and cooperative agreements are no longer necessary as their limited purpose has run out.”
Since the public health emergency for COVID-19 was declared over in the US on May 11, 2023, over 92,000 Americans died from the pandemic virus, according to CDC data. In total, the pandemic killed over 1.2 million in the US.
RFK Jr. claws back $11.4B in CDC funding amid wave of top-level departures Read More »