Man’s health crashes after getting donated kidney—it was riddled with worms
About two months after receiving a donated kidney, a 61-year-old man ended up back in the hospital. He was tired, nauseous, and vomiting. He was also excessively thirsty and producing too much urine. Over the next 10 days, things only got worse. The oxygen levels in his blood began to fall. His lungs filled with fluid. He kept vomiting. He couldn’t eat. Doctors inserted a feeding tube. His oxygen levels and blood pressure kept falling. He was admitted to the intensive care unit and put on mechanical ventilation. Still, things kept getting worse.
At that point, he was transferred to the ICU of Massachusetts General Hospital, where he had received the transplant. He was in acute respiratory failure and shock.
In a case report in this week’s issue of the New England Journal of Medicine, doctors at Mass General explained how they determined what was wrong with the man. Their first steps were collecting more information about the man’s symptoms from his wife, reviewing his family medical history, and contacting the regional organ-procurement organization that provided the kidney.
Process of elimination
The man’s condition and laboratory tests suggested he had some sort of infection. But as a transplant recipient who was on a variety of immunosuppressive drugs, the list of infectious possibilities was “extensive.”
Dr. Camille Kotton, Clinical Director of the hospital’s Transplant and Immunocompromised Host Infectious Diseases division, laid out her thinking. She started with a process of elimination. As an immunosuppressed transplant patient, he was also on several medications to proactively prevent infections. These would rule out herpesviruses and cytomegalovirus. He was also on a combination of antibiotics that would rule out many bacterial infections, as well as the fungal infection Pneumocystis jirovecii that strikes the immunocompromised and the protozoan parasite Toxoplasma gondii.
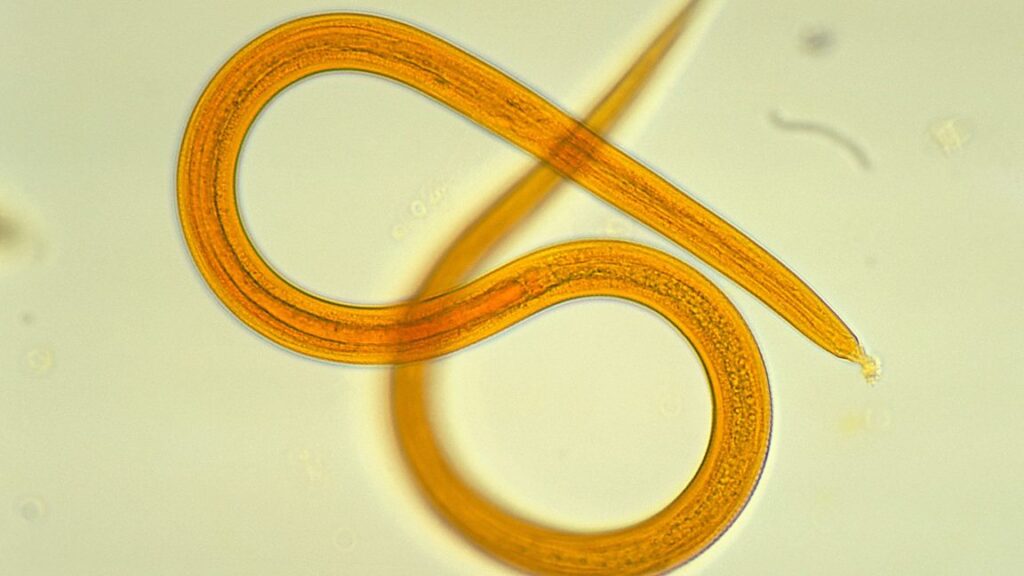
One feature stood out: The man had developed elevated levels of eosinophils, white blood cells that can increase for various reasons—including parasitic infections. The man also had a reddish-purple rash over his abdomen. Coupled with the severity of his illness, Kotton suspected a widespread parasitic infection.
The man’s history was notable for contact with domestic cats and dogs—including a cat scratch in the time between having the transplant and falling critically ill. But common bacterial infections linked to cat scratches could be ruled out. And other parasitic infections that might come from domestic animals in the US, such as toxocariasis, don’t typically lead to such critical illnesses.
Man’s health crashes after getting donated kidney—it was riddled with worms Read More »