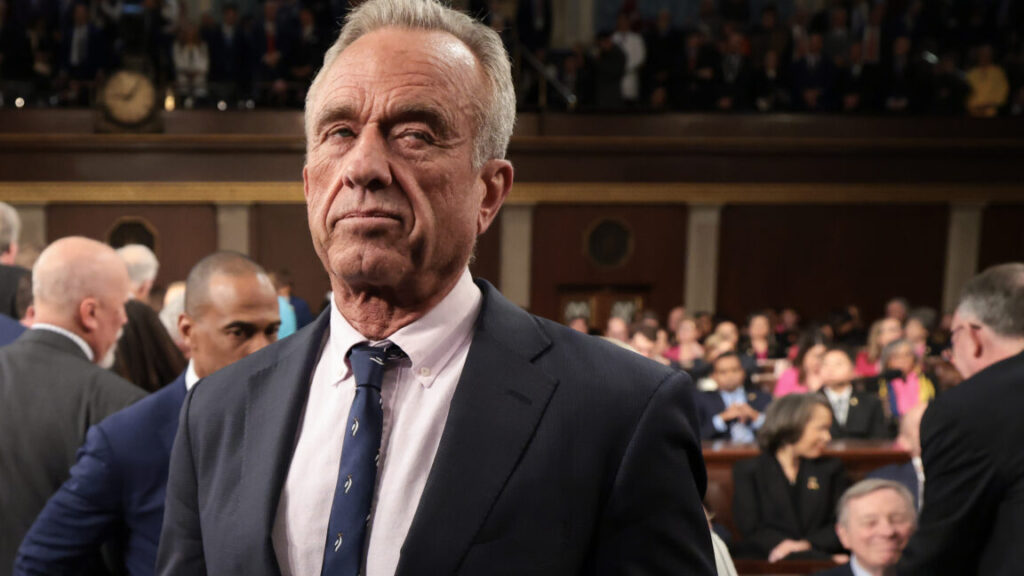
Report: mRNA vaccines are in RFK Jr’s crosshairs; funding in question
Ars Technica has reached out to the NIH and HHS for comment and will update this story with any new information provided. The agencies did not respond to comment requests from KFF.
Kennedy’s misinformation
Before becoming the top health official in America, Kennedy had long railed against vaccines, becoming one of the world’s most prominent anti-vaccine advocates and most prolific spreaders of misinformation and disinformation about vaccines. A 2019 study found Kennedy was the single leading source of anti-vaccine ads on Facebook. Kennedy subsequently faced bans from YouTube, Facebook, and Instagram for spreading misinformation.
Researchers directly blame Kennedy and the Trump administration for the attack on vaccine research.
“Kennedy’s war on vaccines has started,” the mRNA vaccine researcher in Philadelphia told KFF.
“There will not be any research funded by NIH on mRNA vaccines,” the scientist in New York similarly told the outlet. “MAGA people are convinced that these vaccines have killed and maimed tens of thousands of people. It’s not true, but they believe that.”
Kennedy has made various statements against vaccines generally, as well as mRNA vaccines specifically. He falsely claimed the vaccine causes severe harms, including causing neurodegenerative diseases, such as Parkinson’s. In 2021, during the height of the pandemic, Kennedy petitioned the Food and Drug Administration to revoke the authorization of COVID-19 vaccines and refrain from approving any future COVID-19 vaccines. A study in 2022, meanwhile, estimated that the vaccines had saved more than 3 million lives and prevented more than 18 million hospitalizations.
The NIH’s recent moves aren’t the first sign that Kennedy will use his powerful position to attack mRNA vaccines. Late last month, Bloomberg reported that HHS was considering canceling a $590 million grant to vaccine-maker Moderna to develop mRNA vaccines against potential pandemic influenza viruses. That includes the H5N1 virus that is currently devastating US poultry and spreading wildly in dairy cows.
An HHS spokesperson told media at the time that “while it is crucial that the US Department and Health and Human Services support pandemic preparedness, four years of the Biden administration’s failed oversight have made it necessary to review agreements for vaccine production.”
It remains unclear what is happening with that grant review. Moderna declined to comment when Ars reached out for any potential updates Monday.
Report: mRNA vaccines are in RFK Jr’s crosshairs; funding in question Read More »