FDA reverses surprise rejection of Moderna’s mRNA flu vaccine
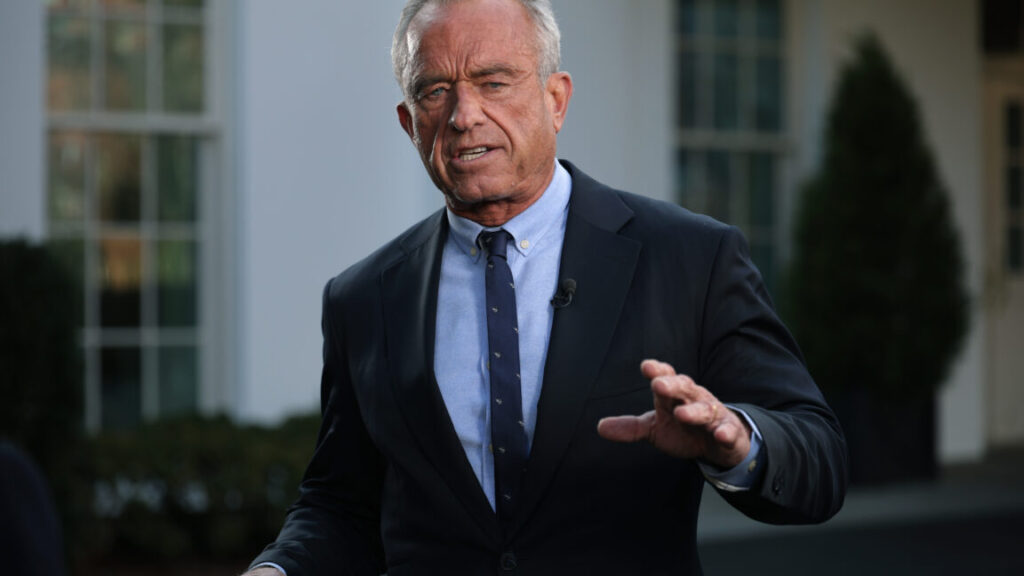
Anti-vaccine agenda
Agency insiders told reporters that a team of career scientists was ready to review the vaccine and held an hourlong meeting with Prasad to present the reasons for moving forward with the review. David Kaslow, a top career official responsible for reviewing vaccines, also wrote a memo detailing why the review should proceed. Prasad rejected the vaccine application anyway.
According to today’s announcement, the FDA reversed that rejection when Moderna proposed splitting the application, seeking full approval for the vaccine’s use in people aged 50 to 64 and an accelerated approval for use in people 65 and up. That latter regulatory pathway means Moderna will have to conduct an additional trial in that age group to confirm its effectiveness after it’s on the market.
Andrew Nixon, spokesperson for the US Department of Health and Human Services, confirmed the reversal to Ars Technica. “Discussions with the company led to a revised regulatory approach and an amended application, which FDA accepted,” Nixon said in a statement. “FDA will maintain its high standards during review and potential licensure stages as it does with all products.”
The FDA typically takes a levelheaded approach to working with companies, rarely making surprising decisions or rejecting applications outright. While Prasad claimed the rejection was due to the control vaccine, the move aligns with Health Secretary Robert F. Kennedy Jr.’s broader anti-vaccine agenda.
Kennedy and the allies he has installed in federal positions are particularly hostile to mRNA technology. Moderna has already lost more than $700 million in federal contracts to develop pandemic vaccines. Next month, Kennedy’s MAHA Institute is hosting an anti-vaccine event that alleges there’s a “massive epidemic of vaccine injury.” The event description claims without evidence that use of mRNA vaccines is linked to “rising rates of acute and chronic illness.”
Vaccine makers and industry investors, meanwhile, are reporting that Kennedy’s relentless anti-vaccine efforts are chilling the entire industry, with companies abandoning research and cutting jobs. In comments to The New York Times, Moderna’s president, Stephen Hoge, said, “There will be less invention, investment, and innovation in vaccines generally, across all the companies.”
FDA reverses surprise rejection of Moderna’s mRNA flu vaccine Read More »