Bird flu jumps from birds to human in Louisiana; patient hospitalized
A person in Louisiana is hospitalized with H5N1 bird flu after having contact with sick and dying birds suspected of carrying the virus, state health officials announced Friday.
It is the first human H5N1 case detected in Louisiana. For now, the case is considered a “presumptive” positive until testing is confirmed by the Centers for Disease Control and Prevention. Health officials say that the risk to the public is low but caution people to stay away from any sick or dead birds.
Although the person has been hospitalized, their condition was not immediately reported. It’s also unclear what kind of birds the person had contact with—wild, backyard, or commercial birds. Ars has reached out to Louisiana’s health department and will update this piece with any additional information.
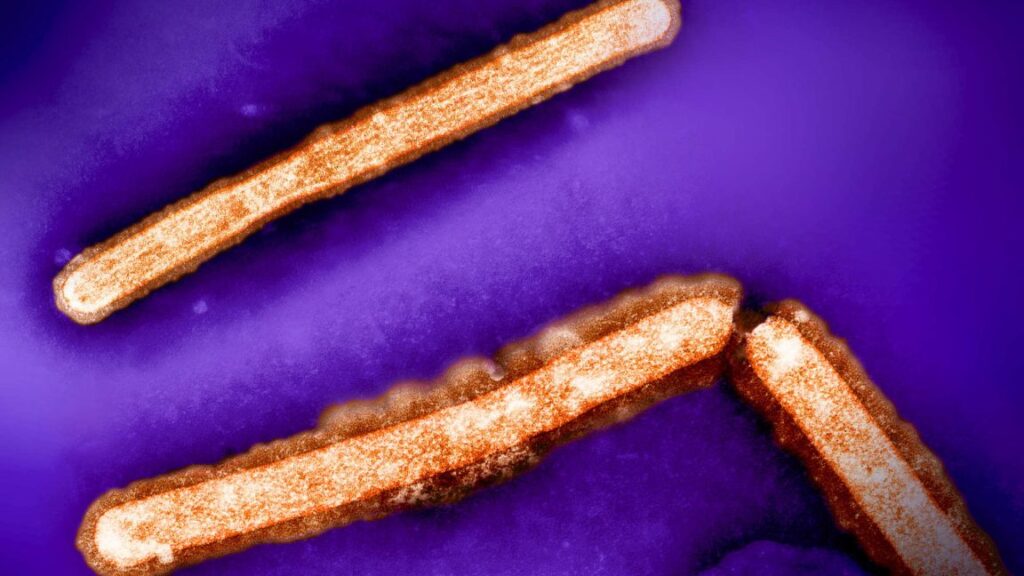
The case is just the latest amid H5N1’s global and domestic rampage. The virus has been ravaging birds of all sorts in the US since early 2022 and spilling over to a surprisingly wide range of mammals. In March this year, officials detected an unprecedented leap to dairy cows, which has since caused a nationwide outbreak. The virus is currently sweeping through California, the country’s largest dairy producer.
To date, at least 845 herds across 16 states have contracted the virus since March, including 630 in California, which detected its first dairy infections in late August.
Human cases
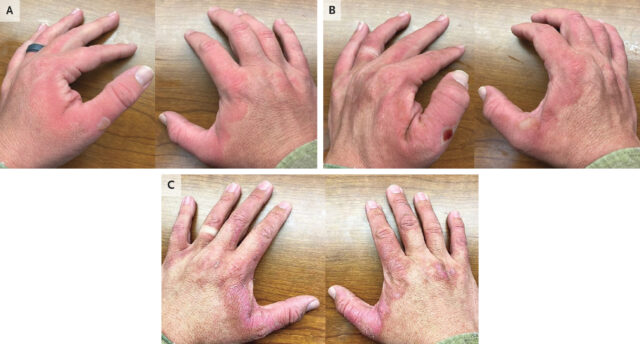
At least 60 people in the US have been infected amid the viral spread this year. But the new case in Louisiana stands out. To date, nearly all of the human cases have been among poultry and dairy workers—unlike the new case in Louisiana— and almost all have been mild—also unlike the new case. Most of the cases have involved conjunctivitis—pink eye—and/or mild respiratory and flu-like symptoms.
There was a case in a patient in Missouri who was hospitalized. However, that person had underlying health conditions, and it’s unclear if H5N1 was the cause of their hospitalization or merely an incidental finding. It remains unknown how the person contracted the virus. An extensive investigation found no animal or other exposure that could explain the infection.
Bird flu jumps from birds to human in Louisiana; patient hospitalized Read More »