Measles continues raging in South Carolina; 99 new cases since Tuesday
The disease usually develops seven to 14 days after an exposure, but it can take up to 21 days (which is the length of quarantine). Once it develops, it’s marked by a high fever and a telltale rash that starts on the head and spreads downward. People are contagious for four days before the rash develops and four days after it appears. Complications can range from ear infections and diarrhea to encephalitis (swelling of the brain), pneumonia, death in up to 3 out of 1,000 children, and, in very rare cases, a fatal neurological condition that can develop seven to 10 years after the acute infection (subacute sclerosing panencephalitis).
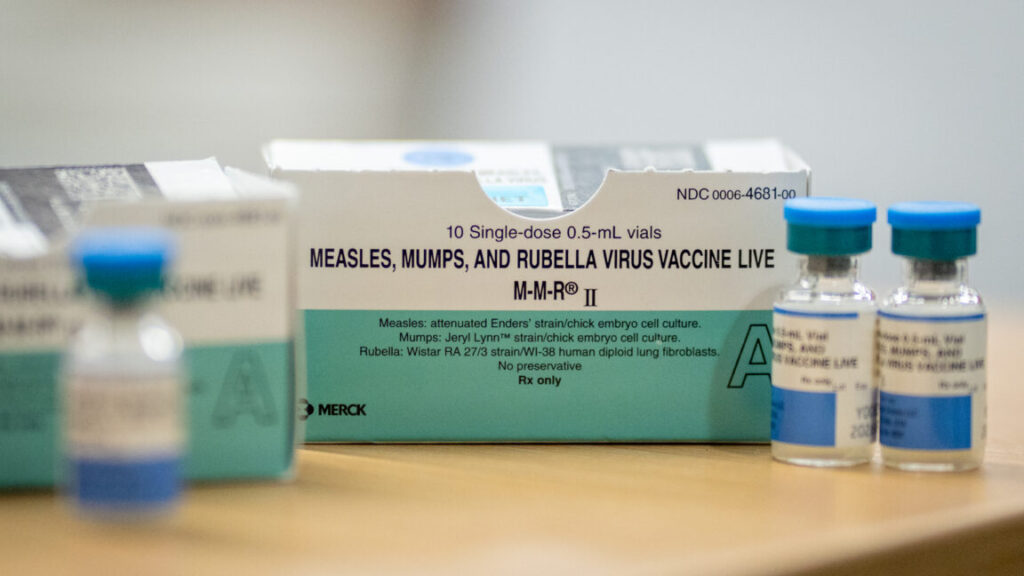
Two doses of the measles, mumps, and rubella (MMR) vaccine is considered 97 percent effective against the virus, and that protection is considered lifelong. Ninety-nine percent of the 310 cases in the South Carolina outbreak are in people who are unvaccinated, partially vaccinated, or have an unknown vaccination status (only 2 people were vaccinated).
The Centers for Disease Control and Prevention, which only has data as of January 6, has tallied three confirmed cases for this year (two in South Carolina and one in North Carolina, linked to the South Carolina outbreak). Since then, South Carolina reported 26 cases on Tuesday and 99 today, totaling 125. North Carolina also reported three additional cases Tuesday, again linked to the South Carolina outbreak. In all, that brings the US tally to at least 131 just nine days into the year.
In 2025, the country recorded 2,144 confirmed cases, the most cases seen since 1991. Three people died, including two otherwise-healthy children. In 2000, the US declared measles eliminated, meaning that it was no longer continuously circulating within the country. With ongoing outbreaks, including the one in South Carolina, the country’s elimination status is at risk.
Measles continues raging in South Carolina; 99 new cases since Tuesday Read More »