Flesh-eating flies are eating their way through Mexico, CDC warns
Across Central America and Mexico, there have been 1,190 human cases of NWS reported and seven deaths. More than 148,000 animals have been affected.
Close calls
In September, the USDA warned that an 8-month-old cow with an active NWS infection was found in a feedlot in the Mexican state of Nuevo León, just 70 miles from the border. The finding prompted Texas Agriculture Commissioner Sid Miller to step up warnings about the threat.
“The screwworm is dangerously close,” Miller said at the time. “It nearly wiped out our cattle industry before; we need to act forcefully now.”
According to the USDA’s latest data, Nuevo León has seen three cases in the outbreak, with none that are currently active. But, its neighboring state, Tamaulipas, is having a flare-up, with eight animal cases considered active. The Mexican state shares a border with the southern-most portion of Texas. Mexico overall has reported 24 hospitalizations among people and 601 animal cases.
For now, the NWS has not been detected in the US, and the CDC considers the risk to people to be low.
“However, given the potential for geographic spread, CDC is issuing this Health Advisory to increase awareness of the outbreak and to summarize CDC recommendations for clinicians and health departments in the United States on case identification and reporting, specimen collection, diagnosis, and treatment of NWS, as well as guidance for the public,” the agency said.
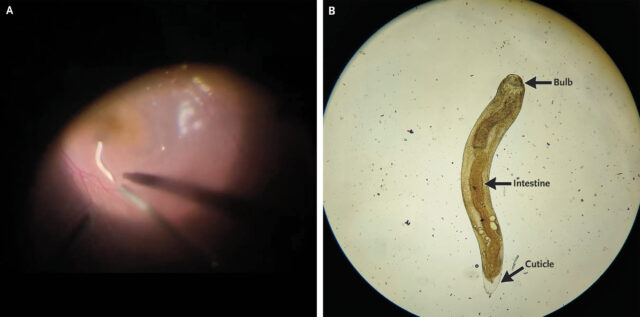
Generally, the agency advises being on the lookout for egg masses or fly larvae in wounds or infection sites, especially if there’s destruction of living tissue or feelings of movement. Once discovered, health care workers should report the case and promptly remove and kill all larvae and eggs, preferably by drowning in a sealed, leak-proof container of 70 percent ethanol. “Failure to kill and properly dispose of all larvae or eggs could result in the new introduction and spread of NWS in the local environment,” the CDC warns in bold. At least 10 dead larvae should then be sent to the CDC for confirmation.
The USDA is currently releasing 100 million sterile male flies per week in Mexico to try to establish a new biological barrier.
This isn’t the fly’s first attempt at a US comeback since the 1960s. In 2016, the flies were somehow reintroduced to the Florida Keys, where they viciously attacked Key Deer, an endangered species and the smallest of North America’s white-tailed deer. The flies were eliminated again in 2017 using the sterile fly method.
Flesh-eating flies are eating their way through Mexico, CDC warns Read More »