RFK Jr. announces 8 appointees to CDC vaccine panel—they’re not good
Anti-vaccine advocate and current Health Secretary Robert F. Kennedy Jr. took to social media Wednesday to announce the names of eight people he is appointing to a critical federal vaccine advisory committee—which is currently empty after Kennedy abruptly fired all 17 previous members Monday.
In the past, the vetting process for appointing new members to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) could take years. But Kennedy has taken just two days.
The panel, typically stocked with vaccine, infectious disease, and public health experts, carefully and publicly reviews, analyzes, and debates vaccine data and offers recommendations to the CDC via votes. The CDC typically adopts the recommendations, which set clinical practices nationwide and determine insurance coverage for vaccinations.
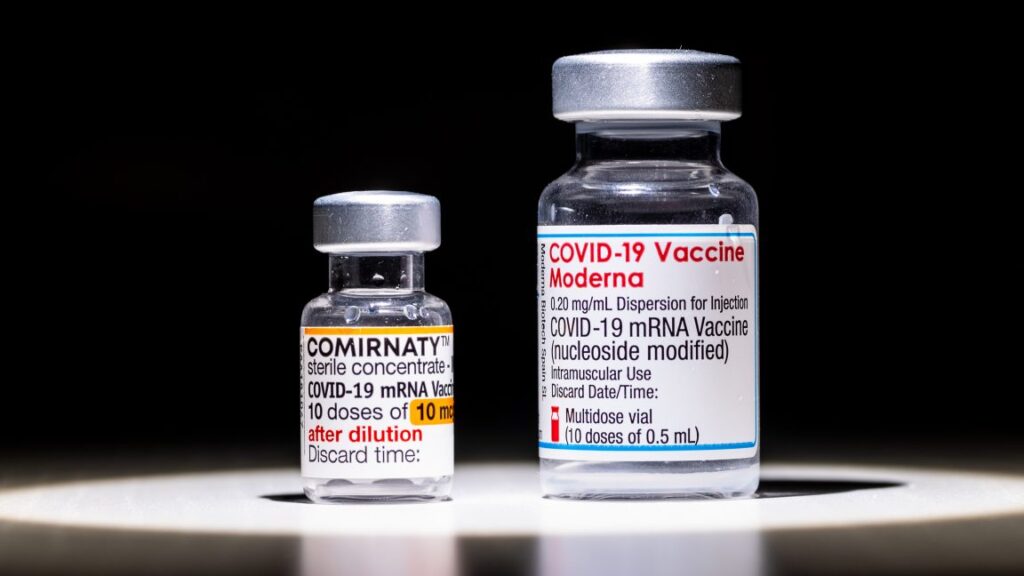
Yesterday, Kennedy pledged that none of the new ACIP members would be “ideological anti-vaxxers.” However, the list of today’s appointees includes Robert Malone, who falsely claims to have invented mRNA vaccines and has spent the past several years spreading misinformation and conspiracy theories about them.
Speaking at an anti-vaccine rally in 2022, Malone spread dangerous falsehoods about mRNA COVID-19 vaccines: “These genetic vaccines can damage your children. They may damage their brains, their heart, their immune system and their ability to have children in the future. Many of these damages cannot be repaired.”
Troubling list
Malone aligned with the anti-vaccine crowd during the pandemic and has become a mainstay in conspiratorial circles and an ally to Kennedy. He has claimed that vaccines cause a “form of AIDS,” amid other nonsense. He has also meddled with responses to the measles outbreak that erupted in West Texas in January. In April, Malone was the first to publicize news that a second child had died from the highly infectious and serious infection, but he did so to falsely claim that measles wasn’t the cause and spread other dangerous misinformation.
RFK Jr. announces 8 appointees to CDC vaccine panel—they’re not good Read More »